Brett Favre Discloses Parkinson’s Disease Diagnosis: Key Information on Symptoms, Causes, and Risk Factors.
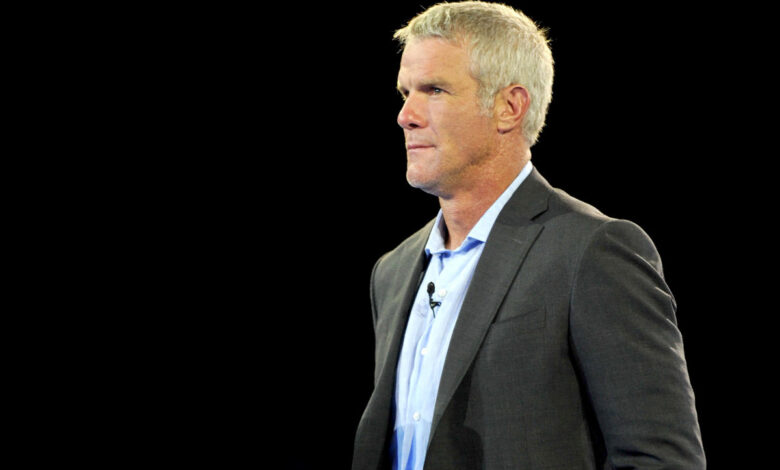
In a startling disclosure that echoes through the hallowed halls of sports and medicine alike, NFL Hall of Famer Brett Favre has recently stepped into the spotlight of a grave personal battle, revealing his diagnosis of Parkinson’s disease on the national stage—an event that unfolded amid a congressional hearing addressing federal welfare reform. The former quarterback, now aged 54, unveiled his diagnosis with a mixture of somber gravity and poignant resolve during deliberations concerning the allocation of Temporary Assistance for Needy Families (TANF) funds, a program that fortuitously funneled millions to Favre’s alma mater, the University of Southern Mississippi, and to Prevacus, a defunct pharmaceutical venture he had championed.
“In an unfortunate twist, I also witnessed the downfall of a venture I had nurtured—one purportedly on the brink of revolutionizing concussion treatment,” Favre shared. “Regrettably for me, while my diagnosis of Parkinson’s stands as a personal milestone, my passion for this cause urges me to fight for others afflicted by similar challenges.”
The illustrious Favre, who electrified the NFL over two decades, previously divulged shocking statistics on The Bubba Army radio show, recounting that he had endured “thousands” of concussions throughout his storied career. He expressed, “Each time my head met the turf, there was a cacophony of ringing and flashing stars—yet I soldiered forth. It’s the seemingly trivial impacts that inflict the deepest damage, as current players grapple with the same fate as I did, perhaps dismissing their own limitations.” Additionally, he has linked his name to a new cinematic venture, Concussed: The American Dream.
Favre’s recent admission has ignited a firestorm of inquiries regarding the nature of Parkinson’s disease and its intricate relationship with concussions. What do neurologists have to say on the matter? Allow us to elucidate.
What is Parkinson’s disease?
This disorienting affliction is a neurodegenerative disorder that manifests through a troubling array of symptoms: involuntary tremors, unyielding stiffness, and precarious coordination or balance issues, as delineated by the National Institute on Aging (NIA). “A noteworthy hallmark of Parkinson’s is the pronounced deceleration in movement,” elaborates Dr. Gian Pal, a premier neurologist specialized in movement disorders at Rutgers Health Robert Wood Johnson Medical School. “Additionally, stiffness, difficulties in maintaining balance, and tremors are prevalent; yet the hallmark remains this sluggishness in motion.”
Notably, this progressive ailment—that actor Michael J. Fox has faced—affects approximately half a million Americans, though the National Institute of Neurological Disorders and Stroke (NINDS) suggests the reality may be far grimmer, with actual numbers potentially eclipsing the official count.
What causes Parkinson’s disease?
The enigmatic origins of Parkinson’s remain shrouded in mystery, with several risk factors surmised to influence its onset. As per insights from Johns Hopkins Medicine, these encompass:
-
Age. Predominantly, the ailment emerges with advancing years, averaging around 60 for diagnosis.
-
Gender. A striking disparity exists, with men finding themselves more susceptible than women.
-
Genetics. Having a lineage of Parkinson’s in the family doubles one’s likelihood of facing a similar fate.
-
Environmental causatives. These factors include exposure to nefarious pesticides, herbicides, heavy metals, and even Agent Orange from the Vietnam War era.
Can concussions elevate your risk for Parkinson’s disease?
The link is a tangled web yet to be fully unraveled. Evidence does suggest a correlation between traumatic head injuries and a heightened risk for Parkinson’s. For instance, research detailed in the journal Neurology posits that even mild brain injuries could elevate one’s risk of Parkinson’s by a staggering 56%. Another study featured in Family Medicine and Community Health corroborates this, indicating those who’ve sustained concussions face a 57% greater likelihood of developing the disease.
“While a connection exists,” suggests Dr. Daniel Truong, neurologist and medical director at MemorialCare’s Truong Neuroscience Institute, “Parkinson’s disease is an intricate beast. A concussion doesn’t guarantee the outcome.” He reiterates the need for more in-depth investigations.
“There’s a correlation between elevated tau protein levels in the brain and Parkinson’s,” expounds Dr. Amit Sachdev, a neurologist at Michigan State University. “Unraveling whether concussion contributes to elevated tau and, subsequently, its role in disease causation is a complex endeavor.”
Pal also references a recent JAMA study highlighting that involvement in football is correlated with an increased probability of receiving a parkinsonism diagnosis—one that exacerbates with the number of years spent on the field. Yet unequivocal clarification remains elusive. “While football participation could be a risk factor,” Pal duly notes, “the body of evidence is still inconclusive.”
Parkinson’s Disease Symptoms
The diverse tapestry of Parkinson’s symptoms varies among individuals, yet the NIA posits four primary manifestations:
-
Tremors in limbs, jaw, or head
-
Muscle rigidity
-
Decelerated movements
-
Instability and coordination issues
Moreover, individuals might grapple with emotional disturbances, difficulties in swallowing, chewing, and communication, as well as urinary and digestive issues, as per the NIA.
How is Parkinson’s disease diagnosed?
Currently, there exist no conclusive blood tests to affirmatively diagnose non-genetic Parkinson’s disease. Medical professionals predominantly rely on medical history coupled with neurological examinations as diagnostic tools. In some scenarios, a brief trial of Parkinson’s medications may be administered to gauge symptom responses, though, as Pal underscores, “this isn’t a requisite for diagnosis.”
Parkinson’s Disease Treatments
“The crux of Parkinson’s disease centers on the brain’s deficits in dopamine—culprit to many of the physical manifestations,” notes Pal. “Fortunately, we have robust treatments available that can replenish this vital neurotransmitter.”
In the preliminary stages, however, it may be that individuals do not require immediate intervention. A collaborative dialogue between patient and doctor typically dictates whether symptoms warrant medication, especially if they impede daily functioning. “It’s a shared decision-making process,” he emphasizes.
Beyond pharmacological approaches, an active lifestyle emerges as a pivotal ally in symptom management, according to Pal.
Should one experience signs indicative of Parkinson’s disease, promptly seeking an evaluation from a specialized movement disorder expert is paramount to discerning if the symptoms signify this condition or an alternative issue. “This can yield crucial insights into the long-term perspective,” he articulates.
“Parkinson’s stands as a progressively entangled disorder,” adds Sachdev, accentuating the necessity of early detection.
Pal remarks that remedies and treatments abound to assist those affected. “Broadly speaking, Parkinson’s is a gradual, progressive condition. Fortunately, a myriad of therapeutic options are at our disposal.”




